Research Illustrates Critical Role 340B Plays for Rural Hospitals and Patients
by David Glendinning | September 7, 2023 3:39 pm
 [1]
[1]Sept. 7, 2023— Recent peer-reviewed research illustrates one of the many ways 340B savings bolster the nation’s rural hospitals and the communities and patients who rely on them for care. The findings help enrich a deep and growing evidence base for the vital role 340B is playing in American health care.
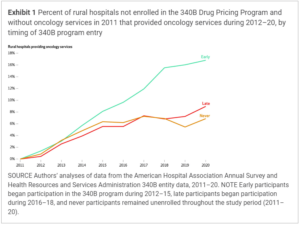
Researchers from the University of Arkansas and the University of Colorado published their findings in Health Affairs[2], one of the nation’s most respected policy journals. The researchers wanted to see whether becoming 340B-eligible led rural hospitals to add critical services to prevent and treat cancer. They focused on rural general acute care hospitals that lacked oncology services in 2011.
340B’s Support for Rural Health
Congress created 340B in 1992 to help hospitals and clinics serving large percentages of low-income patients “stretch scarce federal resources as far as possible, reaching more eligible patients and providing more comprehensive services.” As part of the Affordable Care Act of 2010, Congress voted to expand 340B eligibility to critical access hospitals (CAHs), sole community hospitals (SCHs), and rural referral centers (RRCs), among others. Many of those types of hospitals, which tend to serve rural areas, began to enroll in 2011.
To determine the impact of 340B eligibility on cancer care availability, the researchers looked at three sets of hospitals – the early adopters that enrolled between 2012 and 2015, the late adopters that enrolled in 2016-18, and those that did not enroll. The researchers found the 340B hospitals were 8.3 percentage points more likely to have added oncology services by 2020. “After 340B enrollment there was a clear and persistent increase in the probability of offering oncology services at newly participating hospitals,” the researchers write.
Cancer Care Struggles in Rural America
It has been well-documented in numerous published studies that the 46 million Americans who live in rural parts of the country face significant challenges when it comes to cancer care and prevention. More than 46 million Americans, or 15% of the U.S. population, live in rural areas as defined by the U.S. Census Bureau[3]. Access to cancer care and prevention is especially vital for residents of rural communities, which are often underserved and struggle to gain access to needed care.
The National Cancer Institute[4] has found that rural residents face serious disadvantages compared to urban residents, including socioeconomic deprivation, limited access to quality health care, and risk factors for cancer. While there are many reasons for these disparities, including behavioral and environmental factors, the lack of access to cancer care and prevention is a key factor.
Rural Americans must travel farther to see a cancer specialist. In fact, about one in five rural residents must travel 60 miles or more to obtain care. Because cancer care often requires multiple visits for treatment, rural cancer patients have a harder time accessing and receiving needed treatment.
More Progress Needed
The impact of these disparities is illustrated by research[5] finding that while cancer incidence rates in urban and rural areas are about the same, cancer mortality rates in rural communities are statistically higher. While cancer mortality rates have been dropping in the U.S., a study[6] looking at the annual, age-adjusted mortality rates for all types of cancer during 2006-15 found rates declined more slowly for rural parts of the country (-1.0%) than in urban areas (-1.6%).
The authors of the latest study point to another factor in access to cancer care in rural America. The newly participating hospitals that added oncology services were disproportionately located in Medicaid expansion states and in counties with lower uninsurance rates. The ACA allowed states to expand Medicaid eligibility to include individuals with income up to 138% of the federal poverty line (or a little more than $20,000 a year). According to the Kaiser Family Foundation[7], 40 states and the District of Columbia have adopted the Medicaid expansion and 10 states have not. Most of the states that have not expanded eligibility for Medicaid are in the southeast quadrant of the country, which the American Cancer Society[8] has found to have some of the highest cancer mortality rates in the country.
- [Image]: https://340binformed.org/wp-content/uploads/2023/09/Oncology.png
- Health Affairs: https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2022.01640
- U.S. Census Bureau: https://www.census.gov/library/publications/2016/acs/acsgeo-1.html
- National Cancer Institute: https://gis.cancer.gov/mapstory/rural-urban/index.html
- research: https://www.ruralhealthinfo.org/topics/cancer
- study: https://www.cdc.gov/mmwr/volumes/66/ss/ss6614a1.htm
- Kaiser Family Foundation: https://www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/
- American Cancer Society: https://pressroom.cancer.org/SiegelCancerCD2015
Source URL: https://340binformed.org/2023/09/research-illustrates-critical-role-340b-plays-for-rural-hospitals-and-patients/