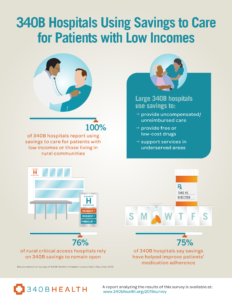
April 2, 2020— Results from 340B Health’s annual survey of hospitals confirms the 340B drug pricing program is working the way Congress intended. Surveyed 340B hospitals report using their savings from prescription drug discounts to improve access to care and health outcomes for patients with low incomes and those living in rural communities. Hospital savings go to maintain or expand patient care, to support the provision of free and discounted drugs, and in the case of rural hospitals, to keep the doors open in an era of frequent closures.
Nearly 500 hospitals participating in the 340B program responded to the survey in November and December of 2019, prior to the beginning of the coronavirus disease 19 (COVID-19) pandemic. The data indicate that 340B savings vary widely based on the size of the hospital. For small, rural hospitals, median savings were $564,000, while the much larger disproportionate share (DSH) hospitals had median savings of $8.9 million. A small number of specialty children’s hospitals surveyed reported higher savings, with a median of $12.6 million.
Hospitals that qualify for 340B status receive discounts when they buy many outpatient prescription drugs to treat patients with cancer, heart disease, diabetes, and other conditions. Congress directed that the savings be used “to stretch scarce federal resources as far as possible, reaching more eligible patients and providing more comprehensive services.” The program, created in 1992, uses no tax dollars to support the care being provided. Savings come from discounts provided by pharmaceutical manufacturers.
Hospitals report using 340B savings in many ways, such as by providing access to free or low-cost drugs, addressing the opioid epidemic, and improving health outcomes for their patients, including through improved medication adherence, better access to care, and reduced readmissions.
A Rural Reliance on 340B
340B plays a special role in the rural communities where one in five Americans live, many at or below the poverty line. Rural hospitals face challenges because of their location in sparsely populated areas distant from urban centers. In 2010, Congress added critical access hospitals (CAHs) to 340B. Such facilities have 25 or fewer beds and are located more than 35 miles from the next nearest hospital. Today, nearly 1,000 such hospitals participate in 340B.
Over the past decade, more than 120 rural hospitals have closed due to financial stresses. In the survey, three-quarters of critical access hospitals report that 340B savings help them stay in operation, and nearly 60 percent report that a loss of 340B savings would put them at risk of closure. More than a third of CAHs use their benefit to support telemedicine programs that provide needed access to specialty care without requiring patients to travel long distances. The use of telehealth has become particularly important during the COVID-19 public health emergency.
More broadly, hospitals report that any loss of 340B savings could force them to make cutbacks to uncompensated care as well as the provision of free or low-cost drugs. Clinical areas that would be most affected by a rollback of 340B include care for cancer, diabetes, mental health and substance abuse, and HIV/AIDS. This year’s survey documents the critical role 340B savings play in providing care for patients in need and reinforces the fact that hospitals continue to fulfill the mission set by the enactment of 340B. Protecting and strengthening this program will continue to bolster the nation’s health care safety net.
Read the report and see our infographic summarizing the key findings.